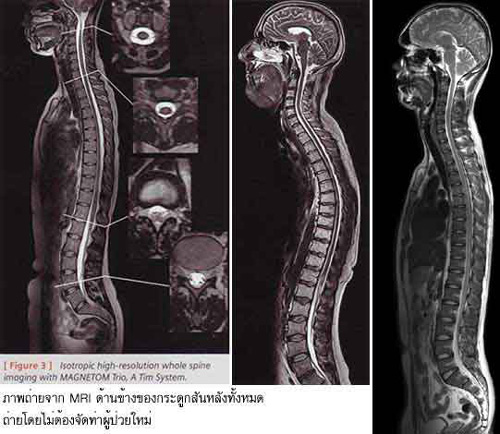
Because MRI can give such clear pictures of soft tissue structures near and around bones.
MRI is usually the best choice for examining the:
- body’s major joints.
- soft tissues of the extremities (muscles and bones).
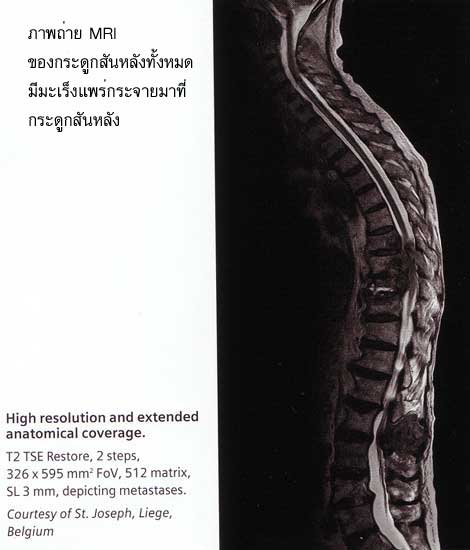
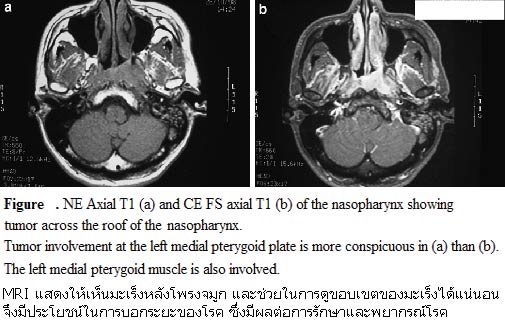
MR imaging is typically performed to diagnose or evaluate:
- degenerative joint disorders such as arthritis and meniscus tears (knee) or labral tears (shoulder and hip).
- locate and identify the cause of pain,swelling or bleeding in the tissues in and around the joints and bones.
- allow the physician to clearly see even very small tears and injuries to tendons, ligaments and muscles that cannot be seen on xrays.
- fractures (in selected patients).
- deterioration of joint surfaces , joint abnormalities.
- sports-related injuries and work-related disorders caused by repeated strain, vibration or forceful impact.
- infections (such as osteomyelitis).
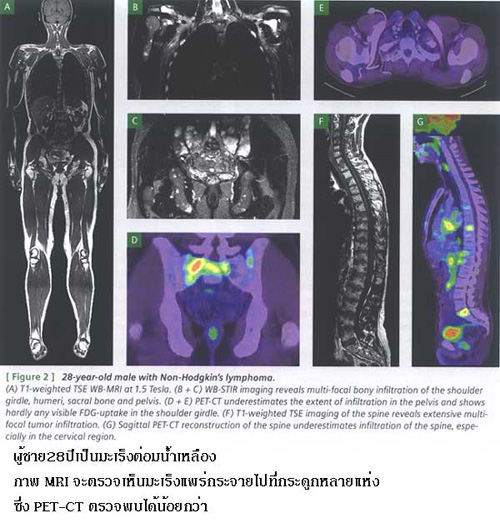
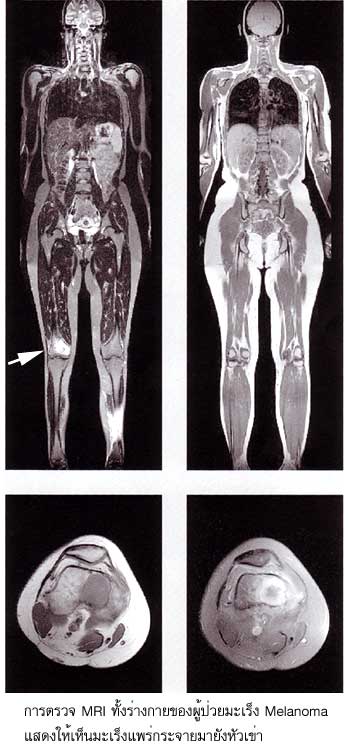
- tumors (primary tumors and metastases) involving bones and joints.
INDICATIONS AND SPECIFIC TECHNIQUES FOR MRI OF THE MUSCULOSKELETAL SYSTEM
Soft Tissues
Spectroscopic fat saturation or short inversion time inversion recovery (STIR) fat suppressed images may be helpful in evaluating soft tissue masses and subtle bone injuries.
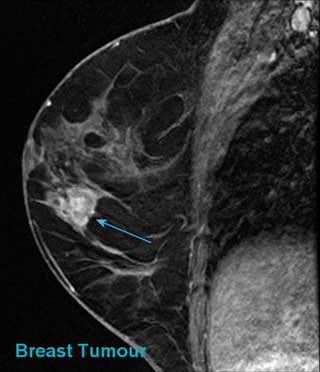
MRI is indicated for the evaluation of traumatic muscle and tendon injuries, hematomas, compartment syndromes , entrapment syndromes, tendinosis, tenosynovitis, and bursitis. MRI is useful for the evaluation of infections, abscesses and myositis. It is indicated for theevaluation of masses such as simple non-neoplastic cysts, abscesses, ganglion cysts, parameniscal cysts, hematomas, muscle tears, and ligament and tendon tears. It is also useful for the detection, staging, and characterization of benign and malignant soft tissue neoplasms and for the follow-up evaluation of neoplastic disease after therapy. (Intravenous contrast agents may be helpful in evaluating potentially malignant disease . For the evaluation of genetic muscle diseases, MR spectroscopy may also be helpful.
Joints
1. Diseases affecting all joints
MRI is indicated for the evaluation of traumatic injuries to joints and adjacent muscles, tendons, and ligaments , selected articular cartilage injuries , bursitis and synovitis from overuse, fragment stability and cartilage status in osteochondritis dissecans , posttraumatic osteonecrosis and degenerative joint disease , loose bodies, and tenosynovitis. MRI is useful in the evaluation of joint infections, noninfectious inflammatory joint disease such as rheumatoid and the seronegative arthritides , overuse synovitis, and tenosynovitis. It is useful for the evaluation of ganglion cysts , bursal cysts with bursitis , abscesses, benign neoplastic masses, and primary and metastatic masses . MRI is indicated for the evaluation of osteonecrosis including avascular necrosis , and degenerative joint disease .
2. Diseases affecting specific joints
- Shoulder
Imaging planes should be selected to coincide with the primary axes of the shoulder. Long TR, double echo coronal images should be obliqued electronically parallel to the supraspinatus muscle or perpendicular to the glenoid fossa of the scapula. (T1W) or (T2W) sagittal images should be obtained perpendicular to the oblique coronal images. Turbo or fast spin echo images are often utilized commonly with fat suppression in the oblique coronal plane. The field-ofview (FOV) should be 12-16 cm. The slice thickness should be less than 5 mm and spatial resolution less than 1 mm. Images in the oblique coronal plane should be acquired with long TR and short and long TE spin echoes such as with a TR of 2,000 msec and TEs of 20 and 80 msec (51). Images in the oblique sagittal plane require contrast adequate for anatomical evaluation, such as TR 500, TE 15 msec or TR 2,000 msec and TEs of 20 and 80 msec. The axial images require good anatomical information as well as images sensitive for fluid. Gradient echo or long TR double spin echo images are adequate in this plane. Acquisition matrices of 192 x 256 are desirable with the number of excitations/averages selected to ensure adequate signal-tonoise.
MRI is indicated for the evaluation of shoulder pain of undetermined etiology, detection and staging of rotator cuff degeneration (tendinosis) and tears, impingement syndromes , labral degenerative changes and tears, biceps tendon disease and dislocation, suprascapular notch syndrome, glenohumeral ligament injuries, coracoclavicular and acromioclavicular separations, subacromial bursitis, and joint anatomy after bony fracture. Suspected instability and labral tears may require intraarticular contrast administration for optimal detection (either MRI after gadolinium chelate or saline injection, or CT arthrography).
- Elbow
Local surface coils and FOV of less than 12 cm are recommended.
MRI is indicated for the evaluation of medial epicondylitis (tennis elbow), fractures in children, osteochondral defects, and osteonecrosis.
- Wrist, Hand, and Fingers
Local surface coils and FOV of 10 cm or less are recommended. Imaging planes should be carefully selected to be in the true coronal, sagittal, and axial planes. Electronic angulation may be necessary to insure proper plane selections. An MR-compatible brace on the wrist may be useful to ensure uniform wrist positioning.
MRI is indicated for the detection and evaluation of the cause of carpal tunnel syndrome, tendon and ligamentous injuries, triangular fibrocartilage injuries, extensor and flexor tenosynovitis, de Quervain’s syndrome , Kienbach’s disease , injuries of the flexor and extensor tendons , tenosynovitis, and masses.
- Hip
Most imaging of the hips is performed without surface coils because of the difficulties of surface coil design for hip anatomy. T1W coronal images are sensitive for osteonecrosis and fractures. T2W images or high-resolution three-dimensional gradient echo images may be useful for evaluating fine anatomical details, especially in children. Subtle bone injuries are common and clinically relevant and may require fat suppressed coronal images for optimal sensitivity.
MRI is indicated for the evaluation of avascular necrosis , congenital hip dislocation, congenital hip dysplasia, transient osteoporosis, and iliopsoas bursitis.
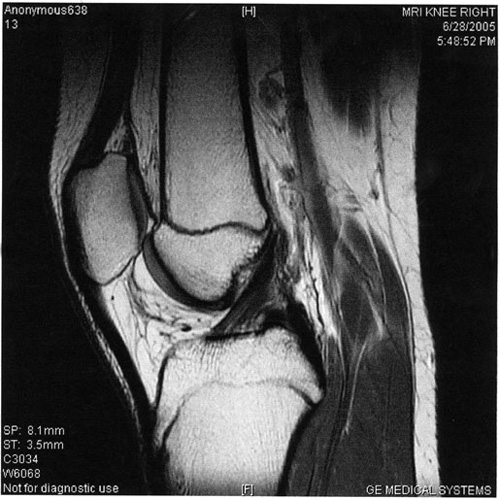
- Knee
Imaging should be performed in at least two planes utilizing at least one (T2W) technique. FOV should be less than 16- cm, pixel dimension less than 1 mm, and slice thickness less than 5-mm. Acquisition matrices of 192 x 256 are advantageous. Magnified, narrow window width display of short TE images containing the menisci may be of benefit in interpretation of meniscal disease.
MRI is indicated for the evaluation of knee pain of undetermined etiology, meniscal tears, discoid menisci, suspected cruciate and collateral ligament tears, bone contusions (trabecular fractures), patellar chondromalacia, patellar tracking abnormalities, popliteal cysts and aneurysmsec, pes anserinus bursitis, prepatellar bursitis, pigmented villonodular synovitis, evaluation of anterior cruciate ligament reconstructions , and meniscal and ganglion cysts.
- Ankle and Foot
FOV less than 12 cm are recommended with appropriately designed local coils. Images should be obtained in the coronal, sagittal, and axial planes with respect to the anatomic region of interest. Suspected disease in the tendons coursing through the ankle may be best evaluated with angled axial images, perpendicular to the tendon at the level of suspected disease. Long TR double echo images and STIR images are advantageous in evaluating tendon and subtle bony injuries. When a tear of the Achilles tendon is suspected, a large FOV sagittal image may be warranted to evaluate the extent of possible retraction of the superior segment. When subtle findings are present, imaging of the contralateral ankle may be helpful.
MRI is indicated for the evaluation of ankle pain of undetermined etiology , tendon and ligament injuries , sinus tarsi syndrome , tarsal tunnel syndrome , plantar fasciitis, masses , postoperative evaluation of Achilles tendon repair , diabetic foot disease , and neurogenic joint disease.
- Temporomandibular Joint (TMJ)
Local surface coils are necessary with FOVs of less than 12-cm. Slice thickness should be 3 mm or less and spatial resolution should be less than 1 mm. Sagittal highresolution (T1W) images are usually performed to determine disc position. If inflammatory disease is present, then long TR, long TE (T2W) images are helpful in evaluating pathology . Kinematic imaging with rapid T1 or gradient echo images may be helpful in characterizing disc placement abnormalities . Since TMJ disease may be bilateral in up to 80% of affected patients, both joints should be imaged, ideally simultaneously .
MRI is indicated for the evaluation of joint pain and clicking , abnormal disc displacement , degenerative joint disease , osteonecrosis of the mandibular condyle , foreign body reaction , inflammatory joint disease , trauma , ganglion cysts , and synovial chondromatosis .